6 Signs You May Have Necrotizing Fasciitis -- Symptoms, Causes, Effects, Treatment and Prevention
Necrotizing fasciitis, also known as flesh-eating bacteria infection, is a severe soft tissue infection characterized by rapidly progressing necrosis (death) of the fascia, subcutaneous tissue, and underlying structures. It is caused by certain bacteria, typically group A Streptococcus or other bacteria like Staphylococcus aureus. Necrotizing fasciitis requires immediate medical attention due to its aggressive nature and potential life-threatening complications.
Symptoms of Necrotizing Fasciitis:
Common symptoms of necrotizing fasciitis include:
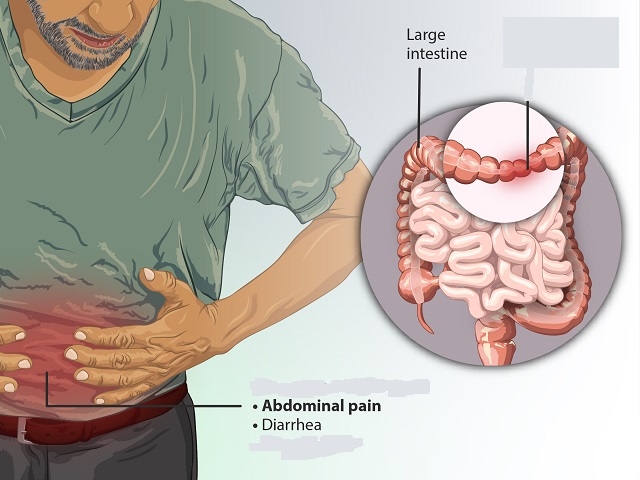
- Severe pain and tenderness in the affected area
- Redness, swelling, and warmth of the skin
- Rapidly spreading skin discoloration or purplish rash
- Blisters, ulcers, or blackened skin
- Fever, chills, and general malaise
- Rapid heart rate and low blood pressure
Diagnosis of Necrotizing Fasciitis:
Diagnosing necrotizing fasciitis involves a combination of clinical evaluation, imaging studies, and laboratory tests, including:
- Physical examination of the affected area
- Imaging tests such as X-rays, ultrasound, or CT scan
- Blood tests to assess markers of infection and inflammation
- Tissue biopsy or culture to identify the causative bacteria
Causes of Necrotizing Fasciitis:
Necrotizing fasciitis is primarily caused by bacteria, most commonly group A Streptococcus (Streptococcus pyogenes). Other bacteria, such as Staphylococcus aureus, Vibrio vulnificus, or Clostridium, can also cause the infection. These bacteria can enter the body through breaks in the skin, surgical wounds, or deep tissue infections.
Effects of Necrotizing Fasciitis:
Necrotizing fasciitis can have severe and potentially life-threatening effects, including:
- Rapid tissue destruction and necrosis
- Systemic infection (sepsis) leading to organ failure
- Complications such as gangrene, abscess formation, or limb loss
- Long-term physical and psychological effects on the affected individual
- Mortality, especially if not promptly diagnosed and treated
Treatment of Necrotizing Fasciitis:
Immediate and aggressive treatment is crucial in necrotizing fasciitis. It usually involves:
- Surgical intervention to remove dead tissue (debridement)
- Intravenous antibiotics to combat the bacterial infection
- Supportive care, including pain management and fluid resuscitation
- Hyperbaric oxygen therapy (in some cases)
- Intensive care management to monitor and stabilize the patient
Prevention of Necrotizing Fasciitis:
Prevention of necrotizing fasciitis involves:
- Prompt treatment of underlying infections, wounds, or injuries
- Proper wound care and hygiene
- Timely medical attention for any signs of infection or skin abnormalities
- Awareness of the risk factors and early recognition of symptoms
References:
Stevens, D. L., Bisno, A. L., Chambers, H. F., Dellinger, E. P., Goldstein, E. J. C., Gorbach, S. L., ... & Wade, J. C. (2014). Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clinical Infectious Diseases, 59(2), e10-e52. doi: 10.1093/cid/ciu444
Hakkarainen, T. W., Kopari, N. M., Pham, T. N., & Evans, H. L. (2014). Necrotizing soft tissue infections: Review and current concepts in treatment, systems of care, and outcomes. Current Problems in Surgery, 51(8), 344-362. doi: 10.1067/j.cpsurg.2014.06.001