4 Signs You May Have Basal Cell Carcinoma -- Symptoms, Causes, Effects, Treatment and Prevention
Basal cell carcinoma (BCC) is the most common type of skin cancer. It typically develops in areas of the skin that are exposed to the sun, such as the face, neck, and hands. Basal cell carcinoma originates in the basal cells, which are located in the lower part of the epidermis, the outermost layer of the skin. It often appears as a raised, pearly bump that may have a central depression or ulceration. BCC grows slowly and rarely spreads to other parts of the body. However, if left untreated, it can cause significant local damage and disfigurement. Here is an explanation of basal cell carcinoma, along with its symptoms, diagnosis, causes, effects, treatment, and prevention:
Symptoms of Basal Cell Carcinoma:
The signs and symptoms of basal cell carcinoma may include:
- Pearly or waxy bump: A translucent or shiny bump that may be pink, red, or white in color.
- Open sore or ulceration: A sore that does not heal or a lesion that bleeds, crusts, or oozes.
- Scar-like area: A white, yellow, or waxy area that resembles a scar.
- Pink growth: A slightly elevated, pink, or red patch of skin that may be itchy or tender.
Diagnosis of Basal Cell Carcinoma:
Diagnosing basal cell carcinoma typically involves a combination of clinical examination and a skin biopsy:
- Clinical examination: A healthcare professional will evaluate the suspicious skin lesion, noting its appearance, size, and any associated symptoms.
- Skin biopsy: A small sample of tissue is taken from the lesion and examined under a microscope to confirm the presence of basal cell carcinoma cells.
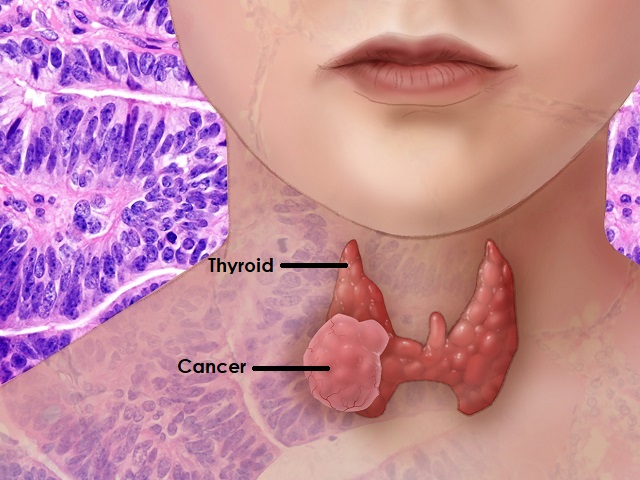
Causes of Basal Cell Carcinoma:
The primary cause of basal cell carcinoma is long-term exposure to ultraviolet (UV) radiation from sunlight or artificial sources, such as tanning beds. Other risk factors include fair skin, a history of sunburns, a weakened immune system, and certain genetic disorders.
Effects of Basal Cell Carcinoma:
If left untreated, basal cell carcinoma can lead to various effects, including:
- Local tissue destruction: BCC can invade surrounding tissues and structures, causing damage and disfigurement.
- Rare metastasis: While rare, basal cell carcinoma can spread to nearby lymph nodes or, in rare cases, to distant organs.
Treatment of Basal Cell Carcinoma:
The choice of treatment for basal cell carcinoma depends on the size, location, and subtype of the tumor. Common treatment options include:
- Surgical excision: The tumor is surgically removed along with a margin of healthy tissue.
- Mohs surgery: This specialized surgical technique involves the sequential removal and examination of tissue layers, ensuring complete tumor removal while minimizing damage to healthy tissue.
- Cryosurgery: The tumor is destroyed by freezing it with liquid nitrogen.
- Radiation therapy: High-energy beams are used to target and kill cancer cells.
- Topical medications: Creams or gels containing medications such as imiquimod or 5-fluorouracil may be prescribed for superficial basal cell carcinomas.
Prevention of Basal Cell Carcinoma:
Preventive measures to reduce the risk of basal cell carcinoma include:
- Limiting sun exposure: Seek shade, especially during peak sun hours, and wear protective clothing, including hats and sunglasses.
- Applying sunscreen: Use broad-spectrum sunscreen with an SPF of 30 or higher on exposed skin.
- Avoiding tanning beds: Artificial UV radiation increases the risk of skin cancer.
It is important for individuals to consult healthcare professionals for accurate diagnosis, personalized treatment plans, and prevention strategies related to basal cell carcinoma.
References:
American Cancer Society. (2021). Basal and Squamous Cell Skin Cancer. Retrieved from https://www.cancer.org/cancer/basal-and-squamous-cell-skin-cancer.html
Leffell, D. J. (2019). Basal Cell Carcinoma. In Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology (8th ed., pp. 601-604). McGraw-Hill Education.
Wong, C. S. M., Strange, R. C., & Lear, J. T. (2020). Basal Cell Carcinoma. In Rook's Textbook of Dermatology (10th ed., pp. 49.1-49.25). Wiley.
Image Attribution:
Featured image by James Heilman, MD, CC BY 3.0, via Wikimedia Commons